In March, Detroit Mayor Mike Duggan declined a shipment of Johnson & Johnson COVID-19 vaccines to Detroit, claiming at a news conference that “I am going to do everything I can to make sure the residents of the city of Detroit get the best.” He also stated that the Pfizer vaccine is better. Following backlash from Detroit residents and negative coverage from news networks, Mayor Duggan backtracked his statements and praised the J&J vaccine.
But this comparison between the J&J and Pfizer vaccines may be indicative of a larger problem: comparing COVID vaccines. Scientists say that there are several reasons why vaccines should not be compared.
A main problem, say scientists, is that people are misreading the efficacy ratings of different vaccines. “The goal of a vaccine was really to defang or tame this virus, to make it more like other respiratory viruses that we deal with, so when you look at the three approved vaccines in the US, all of them are extremely good at that metric,” said Amesh Adalja of the Johns Hopkins Center for Health Security. Pfizer, Moderna, and Johnson & Johnson’s vaccines all showed around 100% efficacy in preventing deaths from COVID-19, and they are also comparable in their ability to prevent hospitalization due to COVID. The J&J vaccine received an efficacy rating of 85.9% in preventing severe cases of COVID-19, compared to the placebo group. “That’s how I think of these vaccines, as basically interchangeable,” said Adalja.
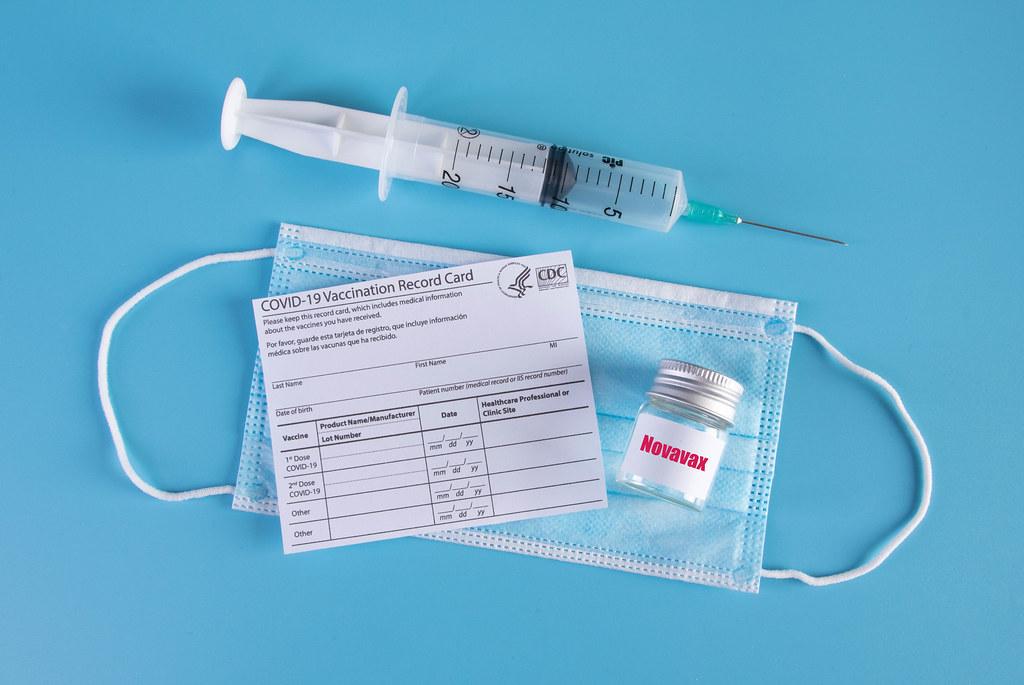
When Johnson & Johnson applied with the FDA for emergency use authorization, it reported an efficacy rating of 66.1%, which worried many people. In comparison, Pfizer and Moderna reported ratings of around 95%. The FDA, for reference, only requires an efficacy rating of 50% for approval. Scientists say that the main reason you can’t compare COVID vaccines is because clinical trials are conducted in different ways, and these methods can result in different metrics being reported.
Many Americans reportedly do not understand what the vaccine efficacy ratings really mean. If a vaccine has 80% efficacy, that does not mean 20% of vaccinated persons will get COVID-19. Rather, it means that the risk of getting the virus is reduced by 80% among the vaccine group, compared to the placebo group. Essentially, if there are 1,000 people in each group, and 20 in the placebo group get the virus, only 4 in the vaccine group would get the virus.
Americans have become familiar with doctor and presidential advisor Anthony Fauci. According to Fauci, one of the leading experts on COVID-19, “If [the announcement of the J&J efficacy rating] had occurred in the absence of a prior announcement and implementation of a 94, 95 percent efficacy [vaccine], one would have said this is an absolutely spectacular result.”
Another reason for the different efficacy numbers is the variation in participants in the trials. Participants have varying levels of access to healthcare. Lockdowns have also been stricter in certain areas than others. The J&J vaccine was also tested in several countries around the world, whereas the Pfizer and Moderna trials employed participants from mostly the U.S. In South Africa, a country where the J&J vaccine was tested and received an efficacy rating of 64%, a new COVID mutation was spreading quickly. The Pfizer and Moderna vaccines were tested earlier, when mutations were far less prevalent. Furthermore, the COVID vaccine trials are not a perfect predictor for how they will perform in the real world. The efficacy numbers are referred to as point estimates, because they only reflect how the vaccines performed in a certain sample size of participants.
Additionally, timing plays a key role. The J&J vaccine finished enrolling participants for their trial in December 2020, one of the worst stages of the pandemic, with infection rates at an all-time high. Pfizer and Moderna, on the other hand, finished enrolling participants in October.
In fact, the J&J vaccine has a few benefits over the other vaccines. First of all, it only requires one dose to achieve immunization. Second of all, it costs less money per dose than Pfizer and Moderna’s offerings, so governments can buy more supply of them. Finally, the J&J vaccine can be stored at more reasonable temperatures, which makes things logistically easier in terms of storage.
Vaccines will be further tested as research continues as to whether they prevent the transmission of COVID-19, as well as whether they prevent against the new mutations emerging throughout the world. For now, scientists say you should get whatever vaccine you can get.